
Blog

Understanding Cushings Disease

Cushing’s disease, also known as Hyperadrenocorticism, is one of the most common hormonal diseases seen in dogs.
Cushing’s disease occurs when the adrenal glands, located just in front of the kidneys,produce too much of the “stress hormone”: cortisol. High levels of circulating cortisol in the blood stream leads to the typical symptoms, which include:
1. Excessive thirst and urination (polydipsia/polyuria) which causes large volumes of dilute urine to be passed.
2. Increased appetite and weight gain.
3. Thin skin and coat, often with hairless patches due to alopecia (hair loss). Often the trunk and tail are the worst affected areas, resulting in a “rat tail” appearance.
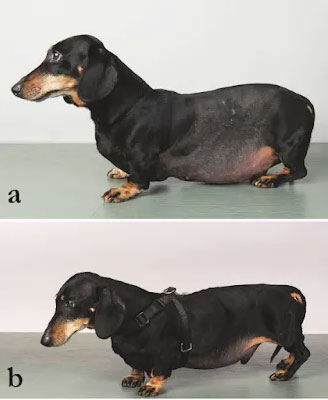
4. Pot-bellied appearance or abdominal distension.
The disease is over-represented in smaller breed dogs such as the Maltese, Shih Tzus and Bichon Frise, (ie. “the white fluffies”) and generally affects middle-aged to senior canines. But it can affect all dogs with high incidence of cases also reported in Beagles, Boxers, Staffies,Dachshunds and Jack Russell Terriers.
What Causes Cushing’s Disease?
There are three main types of Cushing’s disease seen in dogs.
#1. Pituitary Dependent Hyperadrenocorticism (PDH)
This is by far the most common cause of Cushing’s, seen in around 85% of cases. It is caused by a benign tumour of the pituitary gland, which is a pea-sized gland located at the base of the brain. The tumour causes the pituitary to produce an excessive amount of ahormone known as ACTH.
This hormone is responsible for stimulating the adrenal glands to produce cortisol, hence the over-supply of ACTH will result in an over-production of cortisol hormone.
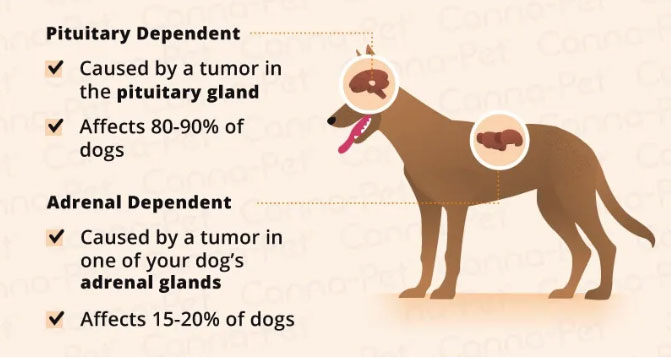
#2. Adrenal Tumour (Adrenal Dependent Hyperadrenocorticism (ADH)
Some unlucky dogs may have Cushing’s disease associated with an adrenal tumour. This tumour stimulates the adrenal glands directly to produce too much cortisol.
Unfortunately, most adrenal tumours in dogs are malignant which means they will spread to other parts of the body. Hence the long-term prognosis will be poor unless aggressive surgery and possibly chemotherapy are undertaken.
Fortunately, adrenal tumours account for less than 15% of total Cushing’s cases.
#3. Iatrogenic Cushing’s
Iatrogenic refers to the inadvertent induction of a disease by medical treatment. In Cushing’s, this is caused by a dog receiving too much steroid medications, for example prednisolone.
Commonly this is seen in patients with severe allergies where no other treatments have been able to alleviate the clinical signs of intense itchiness. Fortunately, this type of Cushing’s is reversible, hence once the animal has been slowly weaned off the medication, the symptoms should resolve gradually.
Diagnosis of Cushing’s Disease:
Definitive diagnosis of Cushing’s disease can be a challenging process because several steps are required:
Step 1: A general blood profile
This will be run if your vet has a clinical suspicion of Cushing’s. For example, if your dog is showing one or more of the clinical signs listed above. There are several other diseases – such diabetes and kidney disease – that can mimic Cushing’s that need to be ruled out first.
This initial test will provide some hints which can include a stress leukogram, raised levels of liver enzymes and higher than normal levels of glucose, cholesterol and albumin.
Step 2: Cushing’s specific bloods tests
Your vet now has 2 options to proceed with:
1. ACTH Stimulation Test
2. Low Dose Dexamethasone Suppression Test or LDDST.
These are both specific tests that measure the body’s cortisol response to certain drugs. They require multiple blood samples to be taken and your pet will need to remain in hospital for 4-10 hours.
Step 3: Abdominal Ultrasound
An ultrasound of the abdomen is a very important part of the diagnostic process. Assessing the size and shape of the adrenal glands will indicate whether it is likely to be Pituitary dependent Cushing’s. In PDH, the adrenals will be bilaterally enlarged but a regular shape (i.e. enlarged to a similar degree on both sides). This is because the excess ACTH hormone causes both adrenals to be affected in the same way.
However, in ADH, the adrenal gland affected by the tumour is likely to be irregular in shape. However, the other adrenal will become small due to hypoplasia. In ADH it is also vital to assess the liver for lesions as this tumour will often metastasize (ie. the cancer will spread) to the liver.

Treatment of Cushing’s Disease:
Trilostane
Treatment will differ according to the type of Cushing’s that has been diagnosed.
The standard treatment for Pituitary-Dependent Cushing’s disease is ongoing medication with Trilostane – a synthetic steroid analogue which blocks cortisol productionand is the standard treatment regime.
The dose required by each patient can be highly variable, so regular follow up blood tests are required to measure the body’s response to the drug, and to inform the veterinarian if dose adjustments need to be made. Trilostane currently needs to be imported from the UK and can prove cost prohibitive for some people.
A slightly older medication, Lysodren or Mitotane, can also be given to treat the disease.
Mitotane works by actively destroying the adrenal tissue, and can be very effective at managing Cushing’s. However, if too little medication is given, the abnormal adrenal tissue remains and the disease will persist.
Conversely, if the dose of medication is too high and too much adrenal tissue is destroyed, this will result in abnormally low cortisol levels. This medical condition is known as Addison’s disease or Hypoadrenocorticism and can be life-threatening, hence careful monitoring with regular blood tests is vital.
Mitotane is generally considered a second line therapy due to its cytotoxic nature which
can be harmful, along with the slightly higher risk of adverse side-effects compared with Trilostane.
Natural remedies including Withania and Dandelion Root can also assist in mild cases of Pituitary Dependent Cushing’s. Some dogs also respond well to a correctly balanced raw food diet.
Surgery option:
In the case of adrenal tumours, a complete adrenalectomy (removal of the adrenal gland) is recommended because the tumour is usually malignant. Due to the close proximity of the adrenal glands to major blood vessels and other vital structures, it is a very involved procedure, and is be best performed by a surgical specialist.
Chemotherapy is generally advised in conjunction with surgery in cases of adrenal tumours.
Prognosis:
Unfortunately, most cases Cushing’s disease cannot be ‘cured’. Management requires ongoing medication and regular monitoring blood tests to achieve a good outcome. The good news is that most dogs suffering from pituitary dependent Cushing’s can be well managed, and most dogs will have a good quality of life with ongoing medication.
Unfortunately, dogs with adrenal tumours have a guarded to poor long-term prognosis as these tumours are often highly aggressive and surgical excision is challenging.
Case Study – “Pepe”

“Pepe” is a white male Miniature Poodle aged 11 years. He was adopted two years ago from the Shenton Park Dog’s Refuge Home of WA and has been quite healthy in this time, however, his medical history prior to adoption is unknown.
I met ‘Pepe’ at his regular annual vaccination booster and health check.
I noticed that his appearance was classic “Cushingoid” with a sparse coat, especially over his trunk and a “rat tail” with barely any hair and thin skin.
Even though his owners had not noticed any of the usual symptoms of Cushing’s, this appearance along with his signalment (a senior, white fluffy breed!) also raised my suspicions.
Pepe’s abdomen felt bloated on palpation but there were no obvious masses nor organ enlargement discernible.
In summary, I found him to be in good general health with no sign of any skin conditions or parasites that would explain the hair loss. I was suspicious of Cushing’s based on these clinical signs andsuspected PDH given the chronicity of the hair loss.
Being over the age of eight, I always recommend an annual health screening blood test, which her owners were happy to proceed with. The initial screening blood work confirmed my suspicion of Cushing’s, showing a stress leukogram, raised liver enzymes and higher than normal levels of cholesterol.
The liver changes could have also been consistent with an age-related nodular hyperplasia of the liver but I was still highly suspicious of Cushing’s and recommended we investigate further with the LDDST.
The LDDST performed definitely diagnosed Cushing’s by demonstrating inadequate suppression of cortisol hormone production after a low dose steroid injection into the bloodstream.
Pepe’s owners are currently deciding which treatment option to pursue but at this stage are the most interested in pursuing treatment with natural remedies.
